Seven toilet training tips that help nonverbal kids with autism
By Dr. Courtney Aponte and Dr. Daniel MruzekThis answer is by psychologists Courtney Aponte and Daniel Mruzek, of the University of Rochester Medical Center, one of 14 sites in the Autism Speaks Autism Treatment Network.
We're looking for help toilet training our 7 year old. He is very limited verbally.
Great question! Many children with autism take longer than is typical to learn how to use the toilet. This delay can stem from a variety of reasons, such as:
- Many children with autism have a general developmental delay. That is, they simply learn new skills more slowly than other children do.
- Many children who have autism have great difficulty breaking long-established routines – in this case using a diaper. Plus, there are relatively few opportunities to practice toileting during the day, as there are only so many times a child genuinely needs “to go.”
- Communication challenges – such as your son’s limited verbal abilities – clearly add to the challenge for many children on the autism spectrum. It’s also common for children with autism to develop anxiety around toileting.
For example, some children with communication challenges won’t understand the question – “Do you need to you use the bathroom now?” Or they may not know how to respond to it or otherwise signal that they need to use the toilet.
Even nonverbal communication can be a challenge among children with autism. In our practices, many parents tell us that their children don’t show the usual signs of an impending accident. For example, crossing their legs, grabbing themselves or even the classic “potty dance.” In other words, these children seem to “go without warning,” making it more difficult for the caregiver to get the child to the toilet in time.
Autism potty training: Strategies to help nonverbal kids
The good news is that we’ve found a number of strategies that help children with autism overcome their toilet training challenges. Before we delve into them, we want to remind you of a very helpful resource and reference, the Autism Speaks ATN/AIR-P Toilet Training Tool Kit. Now to our favorite toilet training strategies:
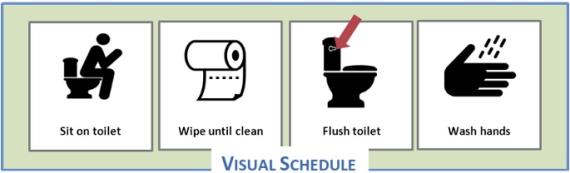
- When it comes to communication: less is more! Use clear and simple pictures or visual prompts such as the visual support below from the Autism Speaks tool kit.
- Use the visual prompt with simple and direct language to help your child understand what is expected. For example, say “Time for potty” instead of asking “Do you need to use the potty now?”
- We’ve found it most effective when parents simultaneously present the verbal direction with the visual support while immediately guiding the child to the toilet with little or no additional discussion.
- Don’t delay the underwear! Move your child into underwear as soon as possible. We realize that this seems an intimidating step for many parents. But we’ve found it’s really important. Let’s face it, modern diapers and pull-ups can be too good at whisking away the pee. As a result, your child may not even realize that he has urinated. Putting your child in underwear helps him associate accidents with the discomfort of wetness on his skin.
- Don’t fuss over accidents. When your child does have an accident, minimize discussing, cajoling, pleading, teasing or other fussing that can have the unintended result of reinforcing the accident behavior. Instead, provide a brief reminder that you expect your child to use the toilet next time he needs to go. Then complete the cleanup with as little fanfare and discussion as possible. Save your attention for when your child is using – or attempting to use – the toilet.
- Reward the desired behaviors. Identify some activities, toys or small treats that will motivate your child. Reserve these for rewarding your child’s toileting successes, and only for rewarding toileting success. Chances are your child will work harder at achieving success if he can’t get these items any other way.
- Importantly, deliver the rewards as soon as possible after your child uses the toilet to pee or poop. Don’t wait! We’ve found that quick delivery of the reward tends to speed skill acquisition.
- And remember those visual supports. For example, you can incorporate a picture of the reward in your child’s toileting visual schedule. OR use a “First-Then” board to illustrate “First use the toilet, and then get your reward.”
- In the early stages of training, reward each small success – even a small dribble of urine. These are important behaviors that you can build upon during subsequent bathroom trips.
- Use rewards to communicate. Sometimes, rewards can help you communicate your expectations to your child. This is especially important for children who have difficulty understanding “if, then” rules.
- For example, your child may not understand, “If you pee in the potty, you can have 5 minutes of iPad.” He may do better if you increase the opportunities for success and reward. How? Try the following:
- On a day you are both at home, increase the fluids he drinks. This will give you more chances to take him to the bathroom for a successful pee. Reward each tinkle!
- Look for patterns in when your child has accidents. It can help to write down the time and place of each accident for several days. You may start to see a pattern emerge. For example, you may find that he often urinates around 30 minutes after drinking a glass of water, milk or other beverage. Use this information to schedule his bathroom trips around times he seems most likely to pee.
- Remember to make those rewards immediate and consistent. This increases the chances that your child makes the connection between peeing and receiving his reward.
- Empower your child to communicate. It’s especially important to help children with limited verbal abilities to signal their need to use the toilet. Once your child is consistently using the toilet when you bring him to the bathroom, it’s time to teach him a simple way to tell you he needs “to go.”
- Consider encouraging him to use a visual support such as a picture of a toilet. Consider clipping it to his belt loop or shirt button hole so he can easily point to it. Or, if your child uses an assisted communication device, you can incorporate a picture of a toilet that he can press to give you an audible cue.
- Ideally, you want him to use these cues when he feels his bladder is full. It can help to slowly stretch out how often you take him to the bathroom unprompted. In other words, you need to give him the chance to recognize what a full bladder feels like – and then experience the relief of peeing in the toilet. As we all know, that relieved feeling can be its own “natural” reward for using the toilet.
- As your child becomes increasingly attuned to when his bladder and bowel is full, he may begin to show more obvious signs of a full bladder. You may start to see an increase in rocking, holding oneself, more vocalizations or other signs that he’s ready for a trip to the bathroom.
- Sometimes a child may simply look intently at you – or toward the bathroom – when he or she needs to go. It’s particularly helpful for parents, teachers and other caregivers to become sensitive to these “tells” and immediately encourage the child to use the chosen communication method. This can be with whatever method works best – e.g., handing you the toilet picture or pressing the toilet button on a speech device.
- Definitely reward your child for any effort to communicate.
- If needed, get professional help. As parents, we often benefit from an expert eye and fresh perspective in what can be a challenging experience for many.
- If toilet training problems persist despite your efforts, we hope you’ll not hesitate getting personalized help from an autism-savvy behavioral therapist or other clinicians.
We hope these autism potty training tips help and we wish you and your son all the best. Thank you for your great question!
Editor’s note: The above information is not meant to diagnose or treat and should not take the place of personal consultation, as appropriate, with a qualified healthcare professional and/or behavioral therapist.